Why Do We Not Have a Vaccine Against HIV or Tuberculosis?
Presenter: Rolf Zinkernagel
Published: July 2014
Age: 18-22 and upwards
Views: 1370 views
Tags: Immune;t-cell
Type: Lectures
Source/institution: Lindau-Nobel
Watch now
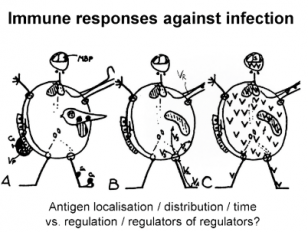
Analysis of the immune system is fascinating and progressing rapidly. As a field of medical enquiry, it has however, drifted and turned purely academic. This is because interest and appreciation of protective immunity in infectious disease medicine has been overtaken by ‘l’art pour l’art’ of so-called ‘basic immunology’. This development deprives much of immunological sciences of the biological basis and understanding that is linked to co-evolution of infectious agents and hosts’ protective immunity. It is this co-evolutionary context that renders this field so different from studying yeast, bacteria, fibroblasts, lymphocytes or neuronal cells in splendid isolation in in vitro model situations, where everything is possible (and permitted or mistakes forgiven without repercussions) because the co-evolutionary context is ignored. I shall explain why we have excellent vaccines against acutely lethal (childhood) infections but not against most slow, chronic persistent infections or tumors, which usually kill us late i.e. after reproduction. Another conclusion is that so-called ‘immunological memory’ of course exists, but only in particular experimental laboratory models measuring ‘quicker and better’ responses, which often do correlate with, but are not the key, mechanisms of protection. Protection depends on pre-existing neutralizing antibodies or pre-activated T cells at the time of infection. This is well documented by the importance of maternal antibodies at birth for survival of offspring. Importantly, both high levels of antibodies in mothers are driven by antigen reencounter. This of course has serious implications for our thinking about old, and hopes for new, vaccines.



